Vision for zero deaths in new-borns
James Temop is a midwife and works as a clinical research assistant in the Division of Health Science at the University of Goroka, Papua New Guinea. In this role, James works closely with nursing and midwifery students who receive clinical skills training at the Goroka Provincial Hospital.
One of the main concerns of the hospital, and Papua New Guinea in general, is the high incidence of newborn deaths: “Infants born before term or at low birth weight are at an increased risk of morbidity and mortality, disrupted growth and development, and are likely to develop chronic disease”, says James. “Lack of cost-effective interventions here contributes to the number of neonatal deaths.”
Background
In 2017, the neonatal mortality rate for Papua New Guinea was 23.7 deaths per 1000 live births, which was the highest in the Oceania region. Recognising this crisis, in 2018 UNICEF introduced a program in Papua New Guinea aiming to reduce the rate of newborn deaths. Goroka Provincial Hospital, located in the eastern highlands, was one of the sites that implemented the program.
To support the initiative, James was sponsored to participate in the JBI Evidence Implementation Training Program in Adelaide to learn about evidence-based healthcare and to develop the skills and knowledge necessary for leading practice change at Goroka Provincial Hospital.
As part of the training program, James led an evidence implementation project that focused on a specific intervention, kangaroo mother care, for improving the outcomes of preterm and low birth weight newborns.

Kangaroo mother care: implementing evidence into practice
“Kangaroo mother care simply involves skin-to-skin contact, chest-to-chest, with a parent – usually the mother”, explains James. Kangaroo mother care has proven effectiveness and is a practical, easy-to-use method for helping to prevent infant deaths. Given that Papua New Guinea has limited resources, kangaroo mother care is an ideal intervention to implement.
Although the UNICEF program introduced at Goroka Provincial Hospital in 2018 included training on kangaroo mother care, and organisational policy supported its implementation, the practice was not widely adopted across the hospital.
In fact, a baseline audit revealed that less than 30% of mothers performed kangaroo mother care. Furthermore, only 20% of healthcare staff received education on the technique, and only about 25% of mothers received education about it. Regular assessment and documentation of infants' condition by healthcare staff was very poor.
“We were disappointed with these results, so we consulted with nursing, midwifery and community health staff to inform them of the results and to gather their perspectives. This strategy of consulting with staff not only provided us with valuable information, but also helped to create a sense of ownership of the project by staff as we worked together to improve compliance for better health outcomes for newborns”.
Based on staff feedback, James and his team developed resources for parents and healthcare practitioners, including handouts, posters, and education programs to increase knowledge and improve adoption of kangaroo mother care.
Training programs for relevant staff were piloted and refined by midwifery tutors from Goroka University. “I was very fortunate to work with a team of academics and nursing/midwifery students from the university, and nursing staff from rural health centres who unselfishly and tirelessly shared their knowledge and skills in making the project successful”, says James.
Barriers and facilitators
Initially, not all staff were enthusiastic about being involved, and some appeared to lack interest. In response, James and his team continued communicating the project's importance, consulting with staff, and involving them in testing educational resources. “We also highlighted that the project was being facilitated by JBI, which everyone considers a leading organisation in evidence-based healthcare. This made staff feel privileged to be part of the project”.
Improving staff understanding of the project's importance and evidence-based healthcare concepts was crucial in overcoming resistance to change.
“Sociocultural norms and adherence to traditional newborn practices were difficult to change at first, even after training. However, ongoing communication and consultation with staff to keep them informed, educated and motivated assisted in achieving widespread change in practice and organisational culture.”
Achieving impact with evidence-based change
A follow-up audit found significant improvements in knowledge and practice of kangaroo mother care among both parents and hospital staff.
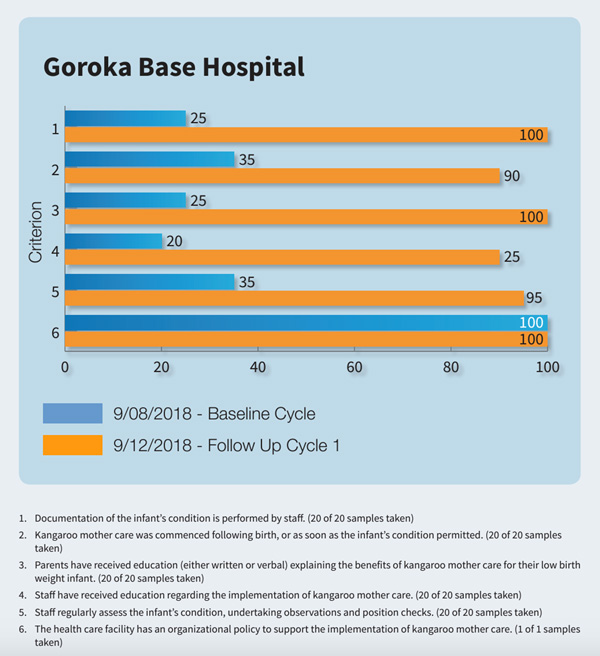
There was a 70% increase in staff receiving education on implementing kangaroo mother care. Additionally, 100% of parents received education on the benefits for their low birth weight infant, a 75% increase from the baseline audit.
Most importantly, instances of kangaroo mother care following birth, or as soon as the infant's condition permitted, increased from less than 30% to 90%.
Additionally, there was a significant increase in adoption of kangaroo mother care by fathers as well as mothers.

“The project was successful in engaging fathers and increasing their involvement in baby care. This was one of the highlights”, says James. This active participation of fathers represents a significant change, as childcare is traditionally considered women's work.
The impact extended beyond parental practices. The project also achieved improvements in assessment and documentation practices by hospital staff. Compliance with assessing, undertaking observations, and position checks of neonatal patients increased by 60%, and documentation of patients' condition increased by 75%.
The positive changes demonstrated in the follow-up audit prove that evidence-based healthcare can be low-cost and implemented successfully with limited resources. Moreover, the project has demonstrated the importance of continued communication and collaboration with key stakeholders to ensure success.
Sustainability of the kangaroo care intervention
Looking forward, James faces the challenge of sustaining this shift in organisational culture and practice to improve care for infants, particularly those born preterm or with low birth weight.
“The project is ongoing”, says James. “The plan is to continue conducting clinical audits and regularly offering educational programs to relevant healthcare staff, so they in turn can educate parents.”

To ensure sustainability, James and his team discussed with the Division of Health Science at the University of Goroka integrating evidence-based healthcare into the curriculum for midwifery and nursing undergraduate students. In 2019, the University hosted a midwifery skills logbook workshop funded by Australia Awards to review and update clinical skills documentation in line with evidence-based practice. This was part of a broader curriculum revision that saw the program transition from a 12-month to an 18-month course meeting International Confederation of Midwives standards for midwifery education.
Scalability
With initiatives such as kangaroo care, Goroka Provincial Hospital has been at the forefront of improving newborn care and saving lives. Building on this success, the hospital trialled a simple medical device called the 'bebi kol kilok' (baby cold clock) worn on an infant's wrist to continuously monitor temperature and alert caregivers if it drops below a safe level. The trial showed the device and associated training were effective in changing behaviours, facilitating decision-making, and encouraging good kangaroo mother care and breastfeeding practice. As a result, recorded hypothermia rates decreased from 21% to 18%. An independent evaluation in 2018 by the US Centers for Disease Control recommended national scale-up of the hypothermia bracelet alongside improvements to newborn care facilities. The Australian Government is supporting this national rollout.
Conclusion
The successful implementation of kangaroo mother care demonstrates that simple, cost-effective practices can dramatically improve neonatal outcomes. James and the Goroka Provincial Hospital team remain optimistic that with their dedication to evidence-based practice and strong partnerships, they will achieve their vision of zero newborn deaths.
Key takeaways
- Actively involving healthcare staff, parents, and academic partners and ongoing communication was essential for overcoming resistance to change and ensuring the intervention's sustainability.
- The effectiveness of the JBI Evidence Implementation Framework in driving meaningful change is demonstrated in this project. Audit and feedback cycles played a pivotal role in identifying practice gaps, tracking progress, and refining interventions such as staff training to improve neonatal care. Continuous improvement cycles led to measurable and lasting impact. Additionally, the Getting Research into Practice (GRiP) method was instrumental in identifying and addressing barriers to change, ensuring the successful integration of evidence-based practices.
- The project's success in improving newborn care highlights the importance of identifying and pursuing opportunities to scale effective interventions, and demonstrates how a targeted initiative can lead to broader, lasting improvements in neonatal health on a national level.
- Actively engaging both mothers and fathers in newborn care, challenged traditional gender roles in the eastern highlands community of Papua New Guinea. This inclusive approach not only improved care practices but also fostered broader sociocultural change in the community for healthier beginnings and brighter futures for babies.
References
CEIC Data. (n.d.). Papua New Guinea mortality rate: Neonatal per 1000 live births.
UNICEF. (n.d.). Australian mammal technique saving lives.
World Health Organization. (2021, May 26). Kangaroo mother care started immediately after birth critical for saving lives, new research shows.
Healthy Newborn Network. (2018). Our baby is my responsibility too: Fathers in Papua New Guinea embrace skin-to-skin contact and relish their new experience.
Post Courier. (n.d.). Kangaroo mother care essential.
University of Technology Sydney. (n.d.). Strengthening nursing and midwifery education in PNG.
International Confederation of Midwives. (2021). Global standards for midwifery education.
Australian Embassy in Papua New Guinea. (2018). EENC and hypothermia bracelet factsheet.
Australian High Commission in Papua New Guinea. (n.d.).
Additional resources
Kangaroo mother care: A practical guide
JBI Manual for Evidence Implementation