Helping babies breathe

Neonatal mortality remains a global challenge. Every year, one million newborns die on the day of their birth, and more than 2.5 million babies die within their first 28 days. Most of these deaths are preventable. According to the World Health Organization, children who die within the first 28 days of birth suffer from conditions and diseases associated with lack of quality care at birth or skilled care and treatment immediately after birth and in the first days of life.
Background
Almost all (98%) of newborn deaths occur in low- and middle-income countries, with 78% of neonatal deaths occurring in Sub-Saharan Africa and Southern Asia. UNICEF estimates that almost 30% of full-term babies who die from birth asphyxia can be prevented, and up to 10% of deaths due to complications of preterm birth can be avoided by effective resuscitation at birth.
Jessie Mwale is a midwifery educator at the Malawi College of Health Sciences, which is situated alongside Zomba Central Hospital, a tertiary and teaching hospital. Around 300 deliveries are made in the hospital’s labour ward every month.

Neonatal data from July 2016 to June 2017 showed that 38% of newborn deaths at Zomba Central Hospital were a result of neonatal asphyxia.
Jessie was sponsored to participate in the JBI Evidence Implementation Program in 2018 and, as part of the six-month program, implemented an evidence-based project to prevent neonatal mortality caused by intrapartum-related asphyxia. "Evidence suggests that deaths from neonatal asphyxia can be prevented and neonatal outcomes can be improved through the training of healthcare practitioners in low-resource settings", says Jessie.
Through a clinical audit and observation studies, Jessie determined that the care of neonates by midwives was not adequate and not well-organised. "Midwives were not prepared for resuscitation. They did not have effective resuscitation skills, and they were not operating in a time-effective manner."
Evidence shows that a newborn’s risk of death increases by 16% for every 30-second delay in initiating ventilation up to six minutes, and 6% for every minute of applied bag and mask ventilation. At the time, however, the midwives did not have the necessary resources readily available, and lacked the knowledge and training to identify and respond effectively to neonatal asphyxia.
Education, training and peer mentoring in evidence-based practice
Jessie used the Helping Babies Breathe program as a framework for educating and training midwives. The Helping Babies Breathe program is an evidence-based educational program designed to teach neonatal resuscitation techniques in low-resource settings.
Essential to the Helping Babies Breathe curriculum is training to respond correctly in the ‘Golden Minute’, the first 60 seconds after birth.
"During the Golden Minute, midwives have the most possibility of positively impacting survival of the newborn babies."
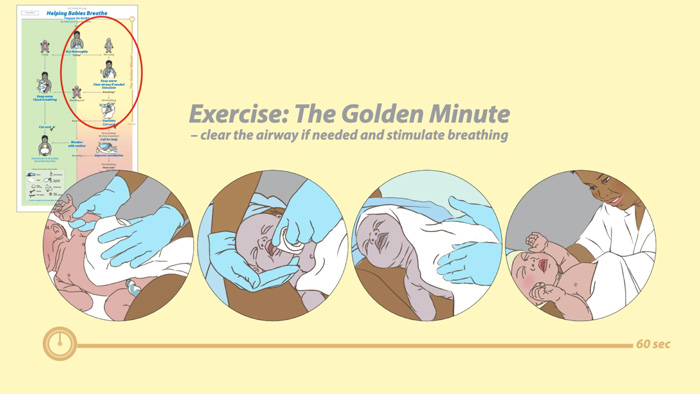
A series of intensive two-day workshops based on the Helping Babies Breathe program curriculum, together with a mentor program for midwives and coordinated peer support for staff, were implemented.
Clinical audit and feedback cycles
The baseline clinical audit revealed that staff lacked the equipment, protocols and guidelines they needed to provide evidence-based care for newborns. Therefore, the latest evidence-based protocols were included in training programs for staff to help ensure compliance with the protocols and the World Health Organization's neonatal resuscitation guidelines.
In addition, equipment was obtained from other hospital departments and external organisations, and government departments were approached to supply equipment. Importantly, a midwife was assigned for every shift to ensure that the emergency equipment for neonatal resuscitation was functional and readily available.
A follow-up audit was conducted six months later, which showed that the project was successful in building the neonatal care competencies of existing staff.
Areas that had been identified as requiring improvement were addressed through the intensive training workshops, including early identification of neonatal asphyxia, timely management of asphyxiated babies and adequate knowledge and skills in resuscitation.

Reducing neonatal mortality: demonstrating impact
Results of the follow-up audit against the baseline audit included:
- 85% of health workers attending deliveries had attended training and maintained competencies in relation to newborn resuscitation;
- an improvement from 48% to 100% of availability of functional equipment and supplies for basic newborn resuscitation in the maternity unit;
- 100% compliance with accurate assessment of newborns and assignment of an APGAR score;
- 90% increase in compliance with managing all newborns with perinatal asphyxia according to the WHO guidelines.
Another audit was undertaken the following year. "The project certainly had an impact", says Jessie. "The hospital data that I obtained for 2019 showed that there was a significant increase in neonatal survival after birth asphyxia. Neonatal mortality from asphyxia decreased to 30% from 38%" This amounts to 21.05% of new born lives saved, including babies born pre-term.
Aligning with United Nations Sustainable Development Goal 3—ensuring healthy lives and well-being for all—Jessie’s evidence implementation project directly advances target 3.2, which is focused on ending preventable deaths of newborns and children under five. Through evidence-based training, enhanced clinical audits, and improved emergency protocols, the program offers a scalable model for reducing neonatal mortality in low-resource settings, and contributing to the global effort to save newborn lives.
Sustainability
Jessie believes that the clinical leadership skills she developed as part of the JBI Evidence Implementation Program played a key role in the project’s success: "The number one thing I learnt from my experience was the importance of engaging and collaborating with clinicians throughout the entire change management process". By engaging staff effectively, giving them responsibilities that contributed to the project’s success and giving them ownership of the project, Jessie also helped to ensure its sustainability.

Scalability
The continuation of peer support and mentor programs, and the provision of intensive training workshops has helped improve and sustain capacity within the labour ward of Zomba Central Hospital so that best practice care of newborns continues. Jessie has continued to further decrease the neonatal mortality rate at the hospital, and even expand the project by working collaboratively with other clinical leaders in Malawi.
Evidence-based initiatives have continued to enhance newborn care at Zomba Central Hospital. These initiatives include NeoTree, which was developed and tested at Zomba Central Hospital. This digital health intervention integrates immediate data capture by healthcare workers on admission with evidence-based clinical decision support and newborn care education. NeoTree aims to provide a guide for diagnosis and management, offering standard management protocols and clinical guidance.
Zomba Central Hospital was also involved in the initial phases of developing clinical decision support algorithms for neonatal care, which were later integrated into the NeoTree. This involved reviewing evidence and guidelines to create algorithms that could support healthcare professionals in the accurate and evidence-based management of neonatal conditions. The groundwork at Zomba Central Hospital was important for the development and iterative refinement of NeoTree as an integrated mHealth solution for newborn care improvement.
Conclusion
The initiative underscores the importance of equipping healthcare workers with the skills and resources needed to save newborn lives. The implementation of evidence-based practices, comprehensive training, and regular clinical audits has led to measurable improvements in neonatal survival rates. Collaborative efforts have strengthened emergency responses and ensured the consistent availability of functional equipment and protocols, while peer support systems have enhanced accountability and continuous learning. These advancements offer a scalable framework for transforming neonatal care in resource-limited settings, ensuring that more babies receive the immediate and effective care they desperately need.
Key takeaways
- Strengthening neonatal resuscitation skills can save lives. Midwives at Zomba Central Hospital gained an understanding of the ‘Golden Minute’ and responded with enhanced skills in neonatal resuscitation, improving their ability to respond quickly and effectively to birth asphyxia.
- Audit and feedback cycles, and regular communication with staff identified barriers to improved neonatal care. Responding with targeted allocation of scarce resources was critical to improved newborn outcomes and enhanced quality of care and underscores that the Getting Research into Practice (GRiP) method can be instrumental in implementing evidence into practice.
- Training and mentorship drive sustainable change. The combination of intensive workshops, peer mentoring, and ongoing clinical leadership helped midwives develop and maintain competencies in neonatal resuscitation and adhere to WHO-recommended neonatal care guidelines, ensuring long-term improvements in care.
References
Ersdal, H. L., Mduma, E., Svensen, E., & Perlman, J. M. (2012). Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low‐income countries: A prospective descriptive observational study. Resuscitation, 83(12), 1423–1428.
UNICEF. (n.d.). Newborn care.
United Nations. (n.d.). Sustainable Development Goal 3: Good health and well-being.
World Health Organization. (n.d.). Newborn mortality.
Additional resources
JBI Manual for Evidence Implementation
Helping Babies Breathe (various languages)