Reducing maternal and neonatal deaths by improving quality of care during labour
Dr Valery Nji in Cameroon implemented evidence-based strategies to improve the quality of care during labour in order to reduce maternal and neonatal morbidity and mortality.
Introduction
According to the World Health Organization (WHO), almost all maternal deaths during pregnancy, delivery or within 42 days of childbirth occur in low-resource settings, and most could have been prevented. Likewise, the rate of neonatal mortality is disproportionately high in low- and middle-income countries. The majority of neonatal deaths are due to preventable causes such as pre-term birth complications, complications during labour and delivery, and infectious diseases such as sepsis.
Cameroon is one of the countries with the highest maternal and neonatal mortality rates. In such settings, the quality of care is paramount, and this includes not only clinical effectiveness but also the experience of care for women. In many countries, including Cameroon, women can experience obstetric violence, which refers to disrespectful, abusive, non-consensual, and neglectful treatment during labour and childbirth at health facilities. This can manifest as unwanted procedures without proper informed consent, verbal or physical abuse, dehumanising treatment, representing a violation of women's human rights. The mistreatment of women giving birth is often delivered verbally and normalised as routine care, removing the opportunity for informed consent.The power imbalance and abuse of trust in the birth space can result in birth trauma, higher rates of postnatal depression, and post-traumatic stress disorder (PTSD).
Background
The World Health Organization recommendations for intrapartum care emphasise that the experience of care is as important as the provision of clinical care for improving quality care for pregnant women during childbirth.
Dr Valery Nji recognised the urgent need to improve the quality of care during labour in Cameroon:
"The World Health Organization provides guidelines for intrapartum care for every woman presenting in labour, but there is little or no compliance in resource-limited settings, mainly due to limited access to these guidelines. Instead, workplace culture and established practice guide the care of these women."

Valery was sponsored by JBI to participate in the Evidence Implementation Training Program and to work closely with JBI research fellows to develop an evidence-based project to identify and implement best practice in the management of pregnant women in labour.
At the time, Valery was based at Bali District Hospital, but the project's viability was threatened by a two-month strike by doctors demanding better working conditions and pay. The strike occurred at a time of political crisis: Anglophone territories in Cameroon’s northwest and southwest had begun declaring independence. This separatist movement resulted in heightened tensions and violent clashes, with both military forces and armed separatists engaging in actions that led to attacks on hospitals. Staff were transferred to St Blaise Catholic Hospital, a mission hospital in rural Cameroon, and the evidence implementation project re-commenced with a clinical audit to determine compliance.

Baseline audit
Criteria for the baseline audit were developed from WHO intrapartum care guidelines, which include non-clinical aspects such as effective communication, respectful care and labour companionship.
"Intrapartum care models that place the healthcare provider as the sole decision-maker in the birth process may expose pregnant women to unnecessary clinical interventions that negatively impact a woman’s childbirth experience. Involving women in the decision-making process, taking into account their preferences and integrating their decisions with clinical experience and best available evidence, can mean a woman’s child-birthing experience is a positive experience."

"Maltreatment of women during labour, be it physical or a failure to reach professional standards of care, is common in resource-limited settings. Developing and implementing a model of provision of continuous support to women during labour will improve outcomes for women and neonates, and decrease negative feelings about the childbirth experience."
Results of the baseline audit revealed that six of the 19 evidence-based criteria showed less than 60% compliance, and one criterion (criterion 9) had zero compliance, ie 'Healthy pregnant women requesting pain relief during labour should be offered pain relief medications'. "The result of 0% compliance against criterion 9 is due to the traditional belief that pains in labour are normal, and that women need no additional pain relief medications", explained Valery.
A criterion for 'Delayed umbilical cord clamping (not earlier than one minute after birth)' had only a slightly higher compliance rate of 6%. "The low compliance rate for criterion 15 is associated with the fear of intrapartum spread of HIV from a woman to her baby. This is despite no evidence showing that early cord clamping reduces the transmission of HIV.
Getting research into practice
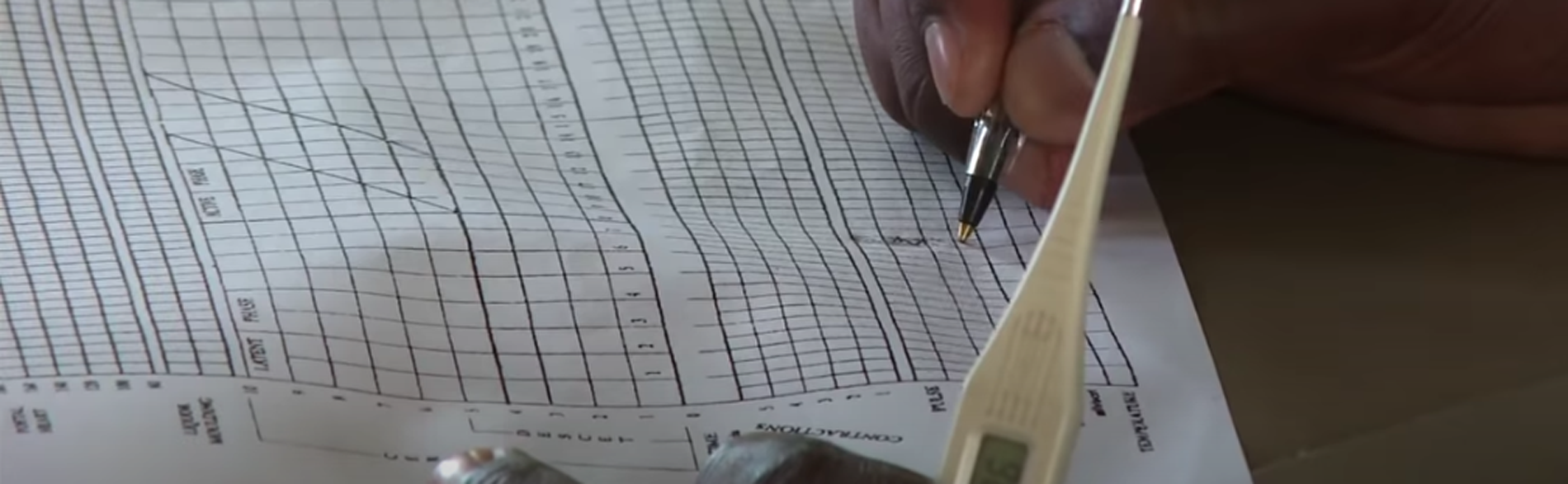
Management of women in labour requires a complete understanding of the mechanisms of labour, a knowledge of medications, and the rationale for labour interventions. It also involves knowing how to use the partogram, considered the gold standard labour monitoring tool. The clinical audit revealed that most practitioners had inadequate knowledge on the current evidence-based guidelines in the management of women in labour. Guidelines were developed and the project team made sure midwives were aware of, and had easy access to, those guidelines.
At first Valery encountered resistance from staff to new practices. The team used the Getting Research into Practice (GRiP) framework to identify and assess barriers to evidence-based practice, as well as strategies and resources required to overcome those barriers. In response, a multi-faceted strategy was employed to educate staff on best practices and the gaps in current practice versus evidence-based guidelines.
Staff were encouraged to engage in the project to gain technical expertise through training - including on the use of the partogram - and as an added incentive, staff actively participating in the project were given a financial stipend.
Follow-up audit results
Results from the follow-up audit, undertaken six months after post implementation of the project, showed that 14 out of the 19 best practice criteria 100% compliance.
For criterion 9, 'Healthy pregnant women requesting pain relief during labour should be offered pain relief medications' compliance improved from 0% to 63%.
For criterion 15, 'Delayed umbilical cord clamping (not earlier than one minute after birth, compliance improved from 6% to 95%.
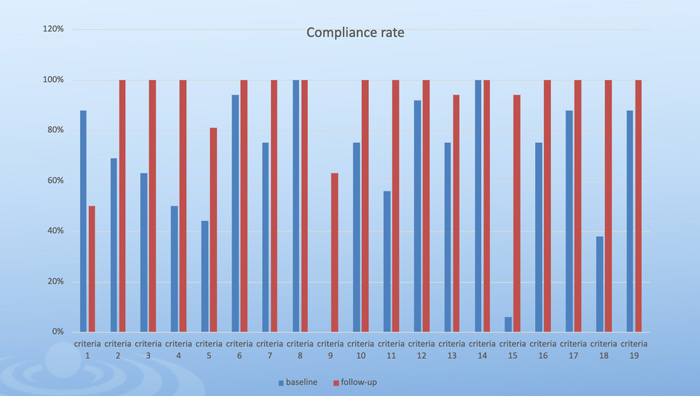
One audit criterion, however, decreased in compliance: 'Effective communication, and respectful maternity care between maternity care providers and women in labour'. Compliance decreased from the baseline value of 85% compliance to 50%. "Follow-up data for criterion 1 were collected from pregnant women after delivery, whereas in the baseline audit, data were collected from the midwives", explained Valery.
"These results show that while the midwives believe they are communicating effectively, their patients think otherwise. The patients wanted to be better informed by midwives about their health throughout their pregnancy and during labour."

Sustainability
The project’s future is one of continuous improvement. Compliance against all guideline criteria is audited every six months, and education strategies for midwives are reviewed, improved and evaluated to help ensure patients’ communication needs are met.
Future directions for the project include expanding beyond St Blaise Catholic Hospital to the greater district so that compliance against evidence-based guidelines informs broader policy. In addition, traditional birth attendants will be encouraged to engage in evidence-based practice and be educated on current guidelines.
"The lack of access to evidence-based criteria by clinicians is especially low in resource-limited settings. This project demonstrates that the non-adherence to evidence-based guidelines which improve maternal and neo-natal mortality and morbidity, and improve the birth experience for women, is a result of limited access to evidence. We successfully improved compliance by making the guidelines available and easily accessed, and by educating clinicians on these guidelines."
Conclusion
According to the World Health Organization, four out of five countries are off track to meet the United Nation’s Sustainable Development Goal 3 target for improving maternal survival by 2030. One in three will fail to meet targets for reducing newborn deaths.
Valery's evidence implementation project can serve as a model for how to improve the quality of maternity care cost-effectively to save lives. Expanding the project beyond St Blaise Catholic Hospital will help hospitals in Cameroon achieve progress towards the United Nation's target for reducing the global maternal mortality ratio to less than 70 per 100,000 live births by 2030, and reducing neonatal mortality. At the same time, reducing obstetric violence and upholding women’s fundamental rights to respectful, person-centred care, ensuring autonomy, dignity, and informed consent, directly contributes to improved maternal health outcomes.
Key takeaways
- In resource-limited settings like Cameroon, maternity care is often guided by ingrained workplace culture rather than up-to-date evidence-based guidelines. Dr. Nji’s project showed that improving access to guidelines and providing practical training (such as on the use of the partogram) significantly enhanced compliance with best practices, leading to better maternal and neonatal outcomes.
- The project emphasised respectful, patient-centred care, including effective communication, informed consent, and shared decision-making during labour. This approach aimed to reduce obstetric violence and birth trauma, promoting dignity and autonomy for women, which is crucial for improving overall childbirth experiences.
- Resistance to change and limited cooperation from healthcare staff were key barriers. The project successfully used a combination of staff education, clear communication of evidence gaps, hands-on training, and incentives to motivate staff, resulting in marked improvements in compliance (from 0% to 63%+ in some criteria).
- Regular audits and continuous staff education are central to sustaining improvements. Plans to expand the project district-wide and involve traditional birth attendants highlight its scalability and potential to influence policy, contributing to global efforts to reduce maternal and neonatal mortality and achieve Sustainable Development Goals (SDG 3).
References
Australian Nursing and Midwifery Federation. (2023). Obstetric violence and birth trauma: Information sheet.
Dalal, A. R., & Purandare, A. C. (2018). The partograph in childbirth: An absolute essentiality or a mere exercise? Journal of Obstetrics and Gynecology of India, 68(1), 3–14.
United Nations. (n.d.). Ensure healthy lives and promote well-being for all at all ages. United Nations Sustainable Development.
World Health Organization. (2024). Strengthening health emergency preparedness in cities and urban settings: Report by the Director-General (EB154/12).
World Health Organization. (2018). WHO recommendations: Intrapartum care for a positive childbirth experience (WHO/RHR/18.12).
World Health Organization. (n.d.). WHO recommendation on effective communication between maternity care providers and women in labour. WHO Reproductive Health Library.
Resources
JBI Manual for Evidence Implementation
Getting Research into Practice (GRiP)
Disclaimer
Republished with permission from World Evidence-based Healthcare Day https://worldebhcday.org/stories/story?ebhc_impact_story_id=68