Reducing the impact of rheumatoid arthritis on people’s lives

Rheumatoid arthritis is a systemic inflammatory disease that affects approximately 0,5% to 1% of the adult population. It is mainly characterised by joint inflammation, which causes pain, swelling and stiffness, and leads, in the long-term, to joint destruction, disability and increased mortality.
The current treatment paradigm of rheumatoid arthritis, epitomised by the treat-to-target strategy, is guided by regular quantified clinical assessments of disease activity and frequent adjustments of therapy aiming at achieving a state of remission as soon and as consistently as possible.
As a result of novel drugs (such as biologics) and the treat-to-target strategy implementation, a marked improvement in the outcomes of rheumatoid arthritis management has been observed regarding both the inflammatory process and the impact of disease. However, a considerable proportion (14% to 38%) of patients with rheumatoid arthritis whose inflammation is in remission still report significant levels of disease impact.
A research team at the rheumatology department at the Centro Hospitalar e Universitário de Coimbra in Portugal proposed the adoption of a dual-target strategy: one focused on the control of the disease process (biological remission) and the other on the abrogation of the disease impact upon patients’ lives. The research team hypothesised that the impact of rheumatoid arthritis upon people’s lives could and should be improved through the introduction of adjunctive interventions targeting the uncontrolled domains of disease impact, especially after remission of the inflammatory process is achieved.
The research team conducted an umbrella review that explored the full potential of adjunctive interventions targeting the different domains of disease impact. As a result of this work, the team was able to identify and characterise all available non-pharmacological interventions by the impact domain of rheumatoid arthritis, thus allowing healthcare professionals to choose and promote interventions targeting the relevant domains in individual patients using a person-centered strategy.
In order to promote the implementation of these interventions in clinical practice, the research team collated the consensus views of clinical experts from a wide range of disciplines and patient representatives into the ‘Portuguese multidisciplinary recommendations for non-pharmacological and non-surgical interventions in people with rheumatoid arthritis’. This publication, which is innovative at a global level, included all relevant scientific societies and patients’ associations from Portugal in this process and endorsed the recommendations.
The research team believes that these contributions may have important implications for a paradigm shift in clinical practice, fostering the ethical imperative of putting the impact of the disease upon patients’ lives at the core of the treatment objectives and management strategies.
There is no doubt that the effective control of the inflammatory process through immunosuppressive therapy must continue to be the cornerstone of the treatment strategy, because rheumatoid arthritis is an aggressive disease that may lead to irreversible structural damage and functional disability.
Furthermore, it is clear that abrogating the disease process makes a substantial contribution to the improvement of virtually all domains of disease impact, including subjective ones like depression, fatigue and sleep.
The research team’s contribution highlights that controlling the disease process does not equate to full abrogation of the disease impact, as endured and reported by a substantial proportion of patients. These patients require additional professional support through adjunctive interventions targeting the domain of persisting impact. To achieve this, healthcare providers need to better understand the impact and promote the full integration of pharmacologic and nonpharmacologic interventions, ideally in the context of a multidisciplinary team. The dual target strategy may have a pivotal role as a framework guide in this endeavor.
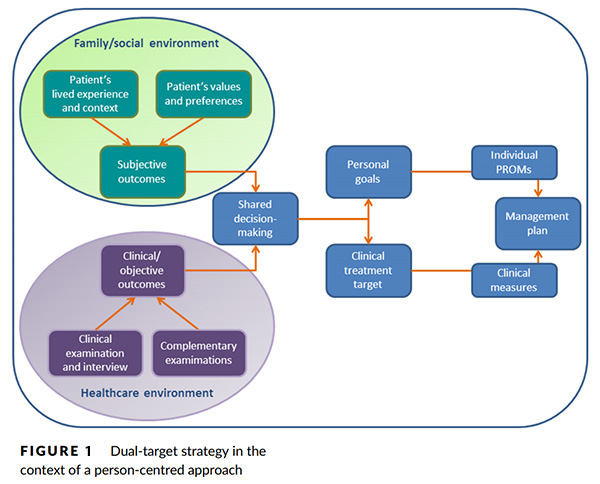
The research team recently developed and proposed a model for this integrative multi-professional effort (Figure 1), departing from its work in rheumatoid arthritis, but potentially applicable to the wider area of chronic disease management. The team looks forward to discussion on the model from the scientific and clinical community.
The research team is now conducting several studies aimed at determining what instruments are best suited to evaluate the impact of disease and to guide disease management. The objective is to provide healthcare professionals with a reliable and meaningful tableau de bord of instruments to help them guide and monitor the management of the disease process, based on the dual target strategy and a strong patient participation.
In the future, the research team will test whether the dual-target approach results in improved outcomes for the patient, although it recognises that this will require a complex approach that can perhaps only be given through a pragmatic randomised clinical trial, based on a priori definitions of appropriate outcomes and interventions.
The research team remains committed to this project and proud to contribute to the improvement of clinical practice and its positive impact upon people's lives.
1. Ferreira RJO, Santos EJF, de Wit M, Marques A, Barbieri-Figueiredo MDC, Marques A, et al. Shared decision-making in people with chronic disease: Integrating the biological, social and lived experiences is a key responsibility of nurses. Musculoskeletal Care. 2020;18:84-91.
Further Resources
Dual target strategy: a proposal to mitigate the risk of overtreatment and enhance patient satisfaction in rheumatoid arthritis
The impact of fatigue in rheumatoid arthritis and the challenges of its assessment
Authors
Eduardo Santos1,2, Maria Barbieri-Figueiredo2,3, José A. P. da Silva1,4
1. Rheumatology department, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal.
2. Portugal Centre for Evidence-Based Practice (PCEBP): A JBI Centre of Excellence, Coimbra, Portugal.
3. Nursing School of Porto, Porto, Portugal, and CINTESIS – Center for Health Technology and Services Research, University of Porto, Porto, Portugal.
4. Coimbra Institute for Clinical and Biomedical Research (iCBR), Faculty of Medicine, University of Coimbra, Coimbra, Portugal.

Eduardo Santos
Disclaimer
Republished with permission from World Evidence-based Healthcare Day October 2020
https://worldebhcday.org/stories/story?ebhc_impact_story_id=87