Reducing the burden of malaria in children under five years of age in Cameroon

Nearly half of the world's population was at risk of malaria in 2023. There were an estimated 263 million cases of malaria, and the estimated number of malaria deaths stood at 597,000. The African Region was home to 94% cases and 95% of malaria deaths. At highest risk for death are children under five years of age, who represent 76% of malaria deaths in the African Region. Malaria is preventable and treatable.
Background
In Cameroon, 71% of the population is at risk of malaria, living in high transmission areas. Malaria is responsible for 50% of hospitalisations in health facilities with 65% of cases being children under five years of age. There were an estimated 7.3 million cases of malaria in 2023, and an estimated 11,600 deaths. Deaths from malaria usually result from complicated malaria; complicated malaria itself is a result of poorly managed uncomplicated malaria.
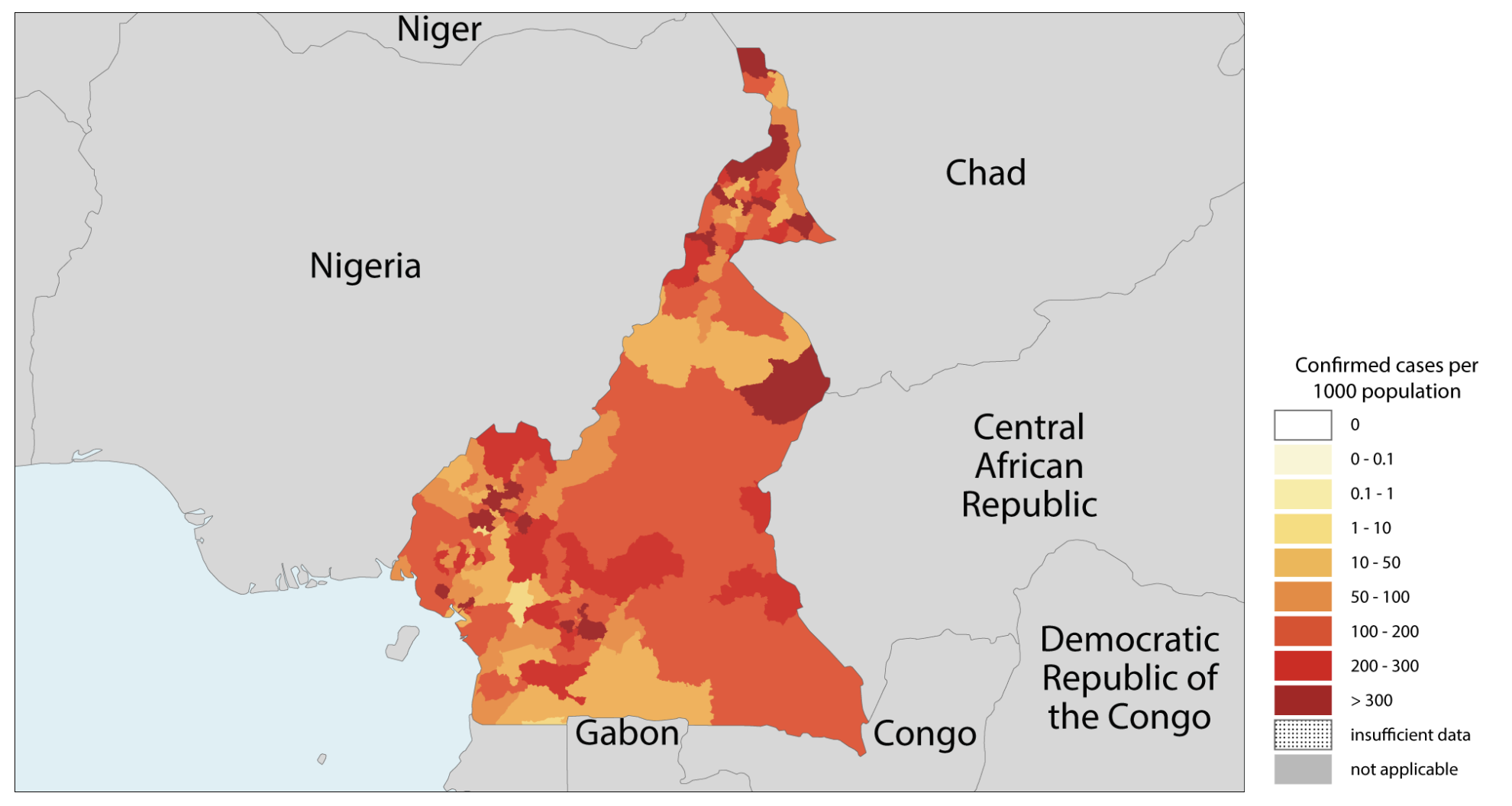
Image courtesy World Health Organization
JBI sponsored Dr Patrick Okwen to participate in the JBI Evidence Implementation Training Program in 2016 to equip him with the skills, knowledge and support to improve the management of uncomplicated malaria in Bali, Cameroon. As part of the program, participants develop an evidence-based implementation project to apply evidence in practice to improve health outcomes in their clinical settings.
"The program builds capacity in the use and implementation of research evidence and clinical leadership, and provides access to evidence summaries, audit criteria and evaluation software", says Dr Okwen.
Promoting artemisinin-based combination therapy
Dr Okwen’s evidence implementation project aimed to promote evidence-based practice in artemisinin-based combination therapy for managing uncomplicated malaria in children under five to improve patient outcomes, and resource utilisation in the Bali Health District.
At the outset of the project, diagnostic and treatment practices were inconsistent with WHO guidelines, contributing to a high burden of complicated malaria. Rapid diagnostic tests were under-utilised, artemisinin-based combination therapy was not consistently prescribed, and health workers lacked clarity and confidence in case management.
"The WHO recommends the use of artemisinin-based combination therapy for the treatment of malaria. Artemisinin-based combination therapy has proven efficacy – it has been shown to significantly reduce morbidity and mortality – and it has good tolerance."
The evidence implementation project followed the JBI Framework for Evidence Implementation, and commenced with engaging stakeholders, establishing a project team and conducting a baseline audit in three health units in the Bali Health District.
Baseline audit
A baseline audit was conducted, using data such as hospital records, patients case notes, laboratory reports and pharmacy reports to measure compliance against five evidence-informed criteria. Results showed compliance against the all criteria at below 60%, with one criterion scoring only 1%:
"Criterion 5: Artemisinin-based combination therapy is prescribed in cases of mixed malarial infections, scored very poorly. Rapid diagnosis tests, while being easy to use, only detect P. falciparum. The audit results for this criterion indicate that clinicians rarely test for mixed infections."
The audit results demonstrated to the project team that management of uncomplicated malaria in children under five was inconsistent and often misaligned with global best practice, contributing to a high burden of complicated malaria. Rapid diagnostic tests were underr-utilised, artemisinin-based combination therapy was not consistently prescribed, and health workers lacked clarity and confidence in case management.
Getting research into practice: identifying barriers and facilitators
Following the baseline audit, results were discussed with stakeholders in the health district, and consultations took place to determine the approach for collectively managing practice change.
"Together, we identified barriers and facilitators to evidence implementation and identified interventions that are feasible, appropriate, meaningful and effective, and which will improve clinical care using the JBI GRiP (Getting Research into Practice) approach."
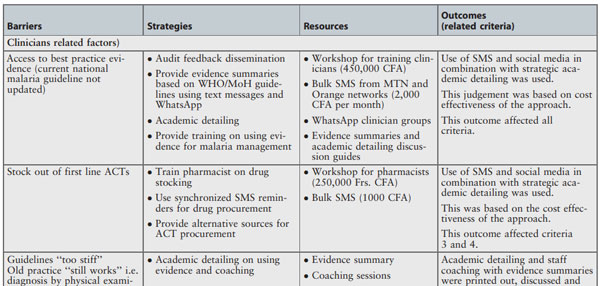
Strategies to overcome barriers included educating and resourcing lab technicians to encourage them to perform microscopy, given the inability of rapid diagnosis tests to distinguish between falciparum species. This meant that mixed malaria could be detected and treated.
Other barriers included parents’ lack of knowledge about the symptoms and management of malaria in children. As a result, an education campaign using talkback radio, social media and SMS was employed.
Follow-up audits
A follow-up audit at all three health centres was conducted as part of the project and demonstrated the project’s success across the three health centres. The aggregated results showed the following improvements in compliance against the evidence-informed criteria:
- Microscopy or rapid diagnosis test is used to confirm the diagnosis in all suspected cases of malaria: improved from 58% to 86%.
- Antimalarial treatment is prescribed to patients on confirmation by positive microscopy and rapid diagnosis test: improved from 40% to 84%.
- Children with uncomplicated malaria are treated with artemisinin-based combination therapy: improved from 49% to 83%.
- A three-day artemisinin-based combination therapy treatment regimen is prescribed: improved from 53% to 93%.
- Artemisinin-based combination therapy is prescribed in cases of mixed malarial infections: improved from 1% to 18%.
Overall, the follow-up audit conducted in December 2017 showed improved compliance with best practice by 31% across the three health centres.
The audit also showed that patient record-keeping and documentation had improved significantly, with missing patient data records reduced by more than 50%.
Evidence to impact
As part of the continuous improvement process, another audit was conducted at all three health centres in 2018. This audit showed that compliance with best practice had improved from 31% to 96.3%.
Importantly, between 2016 and 2019, the number of complicated malaria cases reported in the district decreased by 78%:
"By April of 2019, the national DHIS2 database was reporting Bali as a model district in the case management of malaria in Cameroon, despite political instability and armed conflict in the region."
Sustainability
In order to maintain compliance with best practice, the project team ensured staff are committed to evidence-based practice through regular feedback sessions at district-level coordination meetings. Sustainability was embedded into the initiative through continuous training, routine audits, and the integration of evidence-based practices into district health governance structures. Using the health district as point of entry was helpful in ensuring that the implementation of evidence-based practice for the diagnosis and treatment of malaria could be replicated and rolled-out in other health facilities in the district.
eBASE Africa aimed to deepen and sustain the project's impact further by continuing to address one of the challenges contributing to the high burden of severe malaria in children requiring hospitalisation, which was found during the GRiP phase: parents' lack of knowledge about the symptoms and management of malaria in children.
In 2019, Dr Okwen led an Evidence Hesitancy study, focusing on why caregivers might hesitate to act on evidence-based health information. The study found that community hesitancy was often driven by mistrust, low health literacy, and unfamiliarity with scientific processes. The study team employed traditional forms of communication, ie storytelling, drama, songs, and poetry to communicate the evidence about malaria management in ways that were culturally appropriate and emotionally engaging.
Conclusion
The evidence implementation project has reduced the burden of complicated malaria in children under five. This is mainly due to more uncomplicated cases being correctly managed according to best evidence-based practice before complications set in. The education of parents and caregivers regarding symptoms and management of malaria in children has further contributed to the project's success by addressing root causes of delayed care, such caregiver hesitancy and misinformation.
"The project demonstrates that local leadership and evidence-based care can significantly improve practice in resource-limited settings. As a primary care clinician, I believe the JBI approach to evidence implementation is my best bet to improve clinical effectiveness, improve quality of care, and change workplace culture" says Dr Okwen.
Key takeaways
Evidence-based audits and feedback cycles, when paired with local leadership, can drive sustained, transformative change to help close the research to practice gap.
Identification of barriers and enablers led to targeted interventions that improved compliance with WHO guidelines from 31% to 96.3% over two years.
Effective and targeted communication strategies to engage clinicians and the community was essential to the success and sustainability of the project.
The project, underpinned by the JBI evidence implementation framework, is replicable, adaptable and scalable.
References
RBM Partnership to End Malaria. (n.d.). Cameroon. Severe Malaria Observatory.
World Health Organization. (2024). World malaria report 2024: Cameroon.
Additional resources
Okwen, P. M., Ngem, B., Chia, O. N., Cheabum, R., & Moola, S. (2018). Artemisinin based combination therapy for uncomplicated malaria management among children under five in Cameroon: a best practice implementation project. JBI Evidence Implementation, 16(3), 776–790.
JBI Manual for Evidence Implementation (for GRiP approach and the JBI Evidence Implementation Framework)
World Health Organization. (2024). Cameroon: Malaria country profile 2024.
Disclaimer
This impact story was originally published on the World EBHC Day website: https://worldebhcday.com/impact-stories/reducing-burden-malaria-children-under-five-years-age-cameroon