Improving sleep quality in maternity patients in a Singapore academic hospital

Introduction
Prolonged sleep deprivation and poor sleep quality have negative effects on the physiological and psychological well-being of mothers in the antenatal and postnatal periods, with mothers being at risk of developing postpartum depression and poor emotional coping ability. Sleep disturbances during pregnancy have been associated with pre-term birth, pre-eclampsia, caesarean delivery, gestational hypertension, and gestational diabetes mellitus.
Background
Mothers frequently wake up during the night to provide infant care—such as diaper changes and feeding—thereby further disrupting their sleep. While sleep disruption is an inherent problem among pregnant women and new mothers, the problem is worsened if they are admitted for antenatal monitoring, high-risk complications, or prolonged labour.
In the busy maternity ward at the Singapore National University Hospital, one of Asia's leading medical facilities, expectant mothers often experience interrupted sleep due to the unfamiliar environment, excess light, frequent monitoring, noise exposure, diagnostic tests, and laboratory procedures. Additionally, worry, stress, and fear over their own and their foetus' health may contribute to sleep disturbances.
This was a concern that Tiffany, a senior staff nurse working in the Obstetrics & Gynaecology ward at the hospital, sought to resolve alongside her colleagues Joanne and Shafiqa. These experienced nurses noticed this trend among their pregnant patients and decided to dig deeper. The team searched for the best available evidence on effective sleep promotion strategies using the JBI EBP Database. Key findings from the JBI Evidence Summaries guided their interventions to improve patients' sleep quality. The best practices suggest that reducing noise levels and adjusting lighting may enhance overall sleep quality. Additionally, implementing a multi-faceted approach is recommended for promoting better sleep among patients.
The problem
To identify the practice area for change, the project team surveyed both the nurses and mothers in the maternal ward to determine their perceptions of the main cause of sleep disruption at night-time. The results showed that 56% of mothers and 88.9% of nurses identified night-time procedures (e.g., vital signs monitoring, Cardiotocography (CTG) monitoring the foetal heart activity and maternal uterine contractions, and blood-taking) as the main cause of sleep disruption. Other causes included alarms from medical equipment (identified by 14% of mothers and by 88.9% of nurses). There was a lack of standardised practices and protocols in the ward to guide nurses to promote sleep among the mothers. Having seen first-hand the lack of sleep that the mothers experience while hospitalised, the team embarked on the project with determination with the cooperation of the ward nurses.
Implementing evidence
This project followed the JBI Model of Evidence-based Healthcare and applied the seven phases of the JBI Evidence Implementation Framework. The project team engaged change agents, assessed context readiness, implemented changes, and conducted follow-up audits to measure improvements. The change champions, comprising three nurses and a nurse clinician from the ward, led the project with support from a senior nurse researcher. Their roles included sharing information, developing an audit tool, collecting and analysing data, implementing evidence-based practices, and gathering feedback. The interventions included providing earplugs, reducing alarm volumes, dimming lights, bundling care activities, and adjusting medication administration times where possible.
The team engaged ward nurses and midwives to implement sleep-promoting interventions, through raising awareness about the importance of maternal rest and recovery by sharing evidence on how poor sleep can impact postpartum healing and infant care. Educational sessions were held to inform staff about strategies to minimise nighttime disruptions, such as clustering care activities and using dim lighting. The team collaborated with ward nurses to tailor the intervention, ensuring it was both practical and effective. Clear communication through staff roll-call, posters, and handouts helped reinforce the new practices. Additionally, sleep hygiene information was introduced to mothers, to create a more restful environment. Ongoing feedback was gathered from both staff and patients to refine the approach, ensuring the intervention was sustainable and responsive to the ward’s needs.
Following the project, the multi-faceted approach is now a daily routine for the ward nurses who even take initiative to stock up on ear-plugs without relying on or prompting from project members. This simple action attest to the project team's success in engaging the ward nurses through engagement during roll-call, while on shift, and with visual reminders around the ward.
Demonstrating impact with evidence
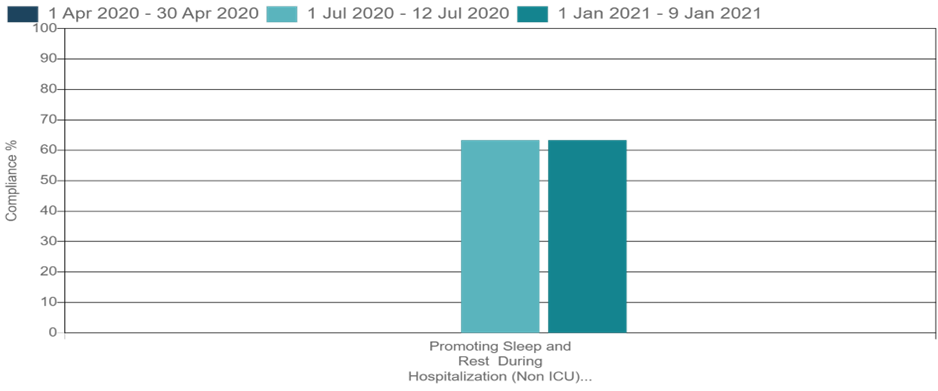
Figure 1: Compliance (%) with best practice for multifaceted approach to sleep promotion audit criterion at the baseline audit, follow-up audit 1 and follow-up audit 2.
The baseline audit showed 0% compliance with best practices for sleep promotion. After implementing the interventions, compliance improved to 63.3% in both follow-up audits (p < 0.01). The mothers’ sleep quality improved, with most reporting that they could sleep longer and felt more alert in the morning. Although the number of night-time wakings remained high, mothers reported being able to fall back asleep more easily. The mothers were fairly satisfied with their sleep quality, and most were able to sleep 4 to 5 hours.
‘’What once required prompting is now second nature — nurses routinely stock earplugs and dim the lights at exactly 9 PM without reminders. These small but consistent actions are powerful indicators of a real mindset shift, showing that the project’s impact has taken root in daily practice.’’
Challenges / lessons learned
“Keeping the ward calm and quiet wasn’t easy with all the work and patients. Sometimes it was hard to remind everyone about the quiet times. But when we saw the mothers resting better, it made the effort worth it.”
During the implementation of the project, ward nurses highlighted several challenges including the lack of earplugs which were not routinely stocked in the ward, fixed medication schedules which could not be adjusted, environmental disturbances such as crying infants and necessary night-time procedures, as well as the introduction of a new infusion pump that did not provide the nurses with the function of lowering alarm sound volumes. Despite these challenges, the education sessions, posters, and materials helped increase nurses’ compliance with sleep promotion strategies, leading to improved patient sleep quality.
Sustainability and next steps
We want every patient in the maternity ward to have a calm and restful space to heal and recover. By lowering noise, dimming lights, and providing earplugs and eye masks, we aim to support better sleep for both mothers and others receiving care. Good rest helps patients feel better, recover faster, and have a more positive hospital experience.
To sustain the best practices, the hospital plans to:
- Conduct regular audits in accordance with the generic guidance on determining the timing of subsequent audits, as recommended in the JBI Manual for Evidence Implementation.
- Continue using posters as visual reminders for nurses and patients.
- Include sleep promotion interventions in staff orientation programmes.
- Work with nursing leaders to ensure the availability of necessary resources such as earplugs.
Key takeaways
- Sleep quality is a crucial aspect of maternal well-being.
- A multi-faceted approach, including environmental modifications and bundled care, can improve sleep quality.
- Nurses’ awareness and engagement play a critical role in implementing sleep-promoting strategies.
- Regular audits and sustainability plans are essential to maintaining best practices.
Conclusion
"I was initially doubtful it would work at first, but now that I see the mothers getting even just a little more sleep than before, it really feels great to know our small efforts have made a real difference"
This project successfully improved compliance with evidence-based interventions for sleep promotion in a maternity ward. While challenges remain, the strategies implemented contributed to improved sleep satisfaction among mothers. Future initiatives will focus on refining interventions based on patient feedback and integrating sleep-promoting strategies into hospital-wide policies for long-term sustainability.
Reference
Lu Q, Zhang X, Wang Y, Li J, Xu Y, Song X, Su S, Zhu X, Vitiello MV, Shi J, Bao Y. Sleep disturbances during pregnancy and adverse maternal and fetal outcomes: a systematic review and meta-analysis. Sleep medicine reviews. 2021 Aug 1;58:101436.
Lee KA, Gay CL. Improving sleep for hospitalized antepartum patients: a non-randomized controlled pilot study. Journal of Clinical Sleep Medicine. 2017;13(12):1445-53.
Marin T, Fong E. Evidence summary. Promoting sleep and rest during hospitalization: non-pharmacological interventions. The JBI EBP Database. 2021; JBI-ES-2529-2.
Woo TML, Lim JSH, Begum S, Goh ML. Improving sleep quality in maternity patients in a Singapore academic hospital: a best practice implementation project. JBI Evidence Implementation.10.1097.
Porritt, K., McArthur, A., Lockwood, C., & Munn, Z. (2023). JBI's approach to evidence implementation: a 7-phase process model to support and guide getting evidence into practice. JBI Evidence Implementation, 21(1), 3-13.
Authors
Tiffany Mei Ling Woo1, Joanne Siew Hui Lim1, Shafiqa Begum1, Mien Li Goh1,2
1. Department of Nursing, National University Hospital, Singapore
2. JBI Singapore National University Hospital Nursing Centre, University of Adelaide, Australia