Evidence-based practice capacity building: a Portuguese experience with undergraduate nursing students

The Nursing School of Coimbra, Portugal, hosts the Health Sciences Research Unit: Nursing (UICISA:E). UICISA:E’s mission is to develop research and development (R&D) activities at an interdisciplinary and international level, with the purpose of providing a sustainable and socially responsible response to complex problems related to health promotion, disease prevention and care delivery to sick, disabled or end-of-life patients. One of the main objectives of the UICISA:E is to carry out R&D activities aimed at synthesising and implementing the best available evidence in order to promote evidence-informed nursing care.
One of the strategic development axes of the UICISA:E is ‘science synthesis and implementation’, and the Portugal Centre for Evidence Based Practice (PCEBP): A JBI Centre of Excellence is a resource for this axis. The mission of this axis is to develop evidence-based practices (EBP) and to work with the international JBI Collaboration on evidence synthesis and implementation. The objectives are to produce systematic reviews following JBI methodology; promote the implementation of evidence into clinical practice; promote training activities in the synthesis and implementation of science; and to disseminate JBI activities.
The PCEBP’s efforts to promote EBP in healthcare began after the centre recognised that EBP prevents unsafe and inefficient practices, and improves healthcare quality. At the same time, the centre recognised that EBP implementation and sustainability are challenging for healthcare organisations and providers. Studies have identified education and training as a strategy to promote EBP implementation, and to close the gap between research and practice.
‘Educating and preparing future nurses in EBP would help minimise the gaps between research and practice, empowering them with research and EBP skills to overcome barriers of EBP implementation, and to become advocates of EBP culture in clinical practice’, says Dr Daniela Cardoso, researcher at the Health Sciences Research Unit.
A team at PCEBP designed a project to integrate EBP into undergraduate nursing curricula within nine nursing education institutions. Using translated and cross-culturally adapted measurement instruments, the team synthesised data on current Portuguese beliefs about EBP and students’ and nursing educators’ levels of implementation knowledge. This evidence was used to develop an educational EBP program.
The program’s effectiveness was evaluated by measuring EBP knowledge and skills in 74 fourth-year undergraduate nursing students at the Nursing School of Coimbra at the conclusion of the project.
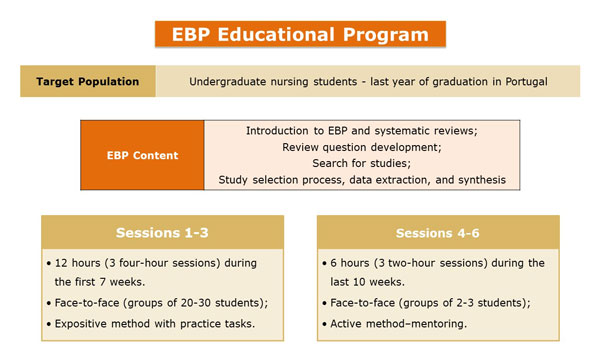
Figure 1. Educational EBP program
‘This project identified that both educators and students had strong EBP beliefs, but a low-level of knowledge of how to implement evidence into practice. Schools have shown a moderate movement to fostering a culture of EBP, which indicates that much more work is required in Portuguese nursing education to achieve an effective EBP culture’, says Dr Cardoso.
The implementation of the educational EBP program contributed to the improvement of EBP knowledge and skills of fourth-year undergraduate nursing students, specifically at the level of review question formulation. Most of the participants of the educational EBP program provided positive feedback on the program:
• ‘The program should last longer and should be extended to all students.’ (‘O programa deveria durar mais tempo e devia estender-se a todos os alunos.’)
• ‘The topics covered were always the most relevant and the best study material was always available. I am grateful for the opportunity to have been part of this program, which allowed me, in the end, to be aware of the work I did, of the mistakes and points that I can improve in the future. In the future, it would be interesting to implement this program for the entire educational community.‘ (‘As temáticas abordadas foram sempre as mais pertinentes e foi disponibilizado sempre o melhor material para estudo. Agradeço a oportunidade de ter feito parte deste programa, que me permitiu, no fim, ter consciência do trabalho que realizei, dos erros e pontos que posso melhorar no futuro. Futuramente seria interessante implementar este programa a toda a comunidade educativa.’)
• ‘Very enriching and useful.’ (‘Bastante enriquecedor e útil.’)
• ‘It was undoubtedly an asset for all students.’ (‘Foi sem dúvida uma mais valia para todos os estudantes.’)
‘Taking into account its contribution to EBP integration in an educational context, it is clear that this research is relevant not only for nursing education, but also for clinical healthcare settings, as building the EBP capacity of student nurses will influence practice, and have a positive flow on effect to healthcare settings in the future’, says Dr Cardoso.
‘Preparing students for the critical use of best available evidence in their future clinical careers will help overcome barriers to implementing EBP in clinical settings and, consequently, will contribute to the promotion and practice of effective healthcare, improve the patient experience and health outcome and reduce health care costs.’
Despite the positive results of the project, the designed and tested intervention was limited in time (17 weeks) and was delivered only to fourth-year undergraduate nursing students, which limits the curricula-wide integration of EBP. Curricula-wide integration of EBP remains a challenge that needs to be addressed by introducing EBP training earlier in undergraduate education. ‘Earlier training in EBP to facilitate the acquisition of EBP knowledge and skills earlier in a student’s education will allow the student to build effective critical thinking skills and consider EBP standard practice, rather than an exception’, says Dr Cardoso.
It has not yet been possible to integrate EBP into undergraduate curricula, however, the PCEBP team has designed a postgraduate course in evidence-informed health care. This postgraduate course will be offered in 2021 and aims to:
• promote advanced training in evidence-informed healthcare for health professionals and researchers, namely in terms of clinical questioning, searching for evidence, critical analysis of evidence, synthesis of evidence and its implementation in daily clinical practice;
• contribute to the training of health professionals so their clinical decision-making is informed by the best scientific evidence.
Further Resources
Cardoso D, Santos E, Cardoso ML, Oliveira CR, Rodrigues MA, Apóstolo J. Instruments for measuring undergraduate nursing students’ knowledge, attitudes and skills in evidence-based practice: a systematic review protocol. JBI Evid Synth. 2017;15(8):1979-86.
Cardoso D, Coelho ARN, da Costa Loucano C, de Oliviera Parola VS, Rodrigues MA, Finout-Overholt E, et al. Translation and adaption of instruments on evidence-based best practice for Portuguese nurisng students [Tradução e adaptação de instrumentos sobre prática baseada na evidência para estudantes de enfermagem portugueses]. Nursing Journal Reference IV Series. 2019;23.
Cardoso D, Fineout-Overholt E, Pereira R, Ferraz L, Rodrigues M, Apóstolo J. Translation, cultural adaptation and preliminary validation of instruments for Portuguese nurse educators on evidence-based practice [Traducción, adaptación cultural y validación preliminar de instrumentos para educadores de enfermería portugueses sobre práctica basada en la evidencia]. The Revista Enfermería Actual en Costa Rica. 2019;38.
Cardoso DRN, Rodrigues MA, Apóstolo J. Evidence-based practice educational program: a Portuguese experience with undergraduate nursing students. JBI Evid Implement. 2019;17:S72-S74.
Authors
Daniela Cardoso1, Manuel Alves Rodrigues1, João Apóstolo1
1. Portugal Centre for Evidence-Based Practice (PCEBP): A JBI Centre of Excellence, Health Sciences Research Unit: Nursing (UICISA: E), Nursing School of Coimbra (ESEnfC), Portugal.

Daniela Cardoso, Manuel Alves Rodrigues and João Apóstolo
Co-publication declaration
This article is based on Daniela Cardoso's PhD thesis presented to the Faculty of Medicine of the University of Coimbra.
Disclaimer
Republished with permission from World Evidence-based Healthcare Day
https://worldebhcday.org/stories/story?ebhc_impact_story_id=102