Congenital and Gestational Syphilis: Evidence Supporting Best Practices

Congenital syphilis is a preventable condition that remains a serious public health issue both in Brazil and globally. When syphilis is acquired during pregnancy, it is referred to as gestational syphilis. If not properly diagnosed and treated, the infection can be transmitted from the mother to the foetus, resulting in congenital syphilis. It is estimated that in 2022, approximately 8 million people were diagnosed with syphilis, with the highest incidence reported in Africa and the Americas. When contracted during pregnancy, the infection can lead to stillbirth, neonatal death, congenital malformations, preterm birth, and low birth weight.
According to the World Health Organization, in 2022 there were an estimated 700,000 cases of congenital syphilis and 390,000 adverse outcomes, including 150,000 early foetal deaths and stillbirths, 70,000 neonatal deaths, 55,000 preterm births or low birth weight cases, and 115,000 infants diagnosed with congenital syphilis. In Brazil, between 1999 and 2024, a total of 344,978 cases of congenital syphilis were reported in children under 1 year of age. In 2023, the country recorded an incidence rate of 9.9 congenital syphilis cases per 1,000 live births and a specific infant mortality rate from congenital syphilis of 7.7 deaths per 100,000 live births.
Context
The state of Mato Grosso, located in the Central-West region of Brazil, is characterised by vast rural areas and significant territorial dispersion. Within this context, obstetric nurse and researcher Prof. Dr. Silvana Benevides Ferreira, a faculty member of the Graduate Program in Nursing at the School of Nursing of the Federal University of Mato Grosso (FAEN/UFMT), leads projects focused on public health and the surveillance of neglected diseases.
In collaboration with her master's and doctoral students—who are also practising clinical nurses—she conducts research on integrating scientific evidence into clinical practice. As Silvana emphasises, ‘The increase in syphilis infections can be attributed to multiple factors, including a lack of awareness about the disease, difficulties in accessing healthcare services, delayed diagnosis and treatment, as well as the persistent stigma surrounding sexually transmitted infections.’
Within this scenario, nursing plays a crucial role on the front lines of healthcare, often serving as the first point of contact for pregnant women accessing health services. Brazil's Unified Health System (SUS) is the main pathway for access to free healthcare. In 2024, 48,272 initial prenatal care visits were recorded in the state of Mato Grosso. In this setting, the important role of nursing care is clearly reflected in the testimony of a pregnant woman who was diagnosed with gestational syphilis, ‘I was diagnosed with syphilis early in my pregnancy. Although I had heard of the disease, the diagnosis frightened me. The first thing I thought about was the risk to my babies. At first, I must admit I felt a sense of stigma—not directly from the professionals, but from the stigma that this disease carries, especially for us women. Fortunately, I was very well received by the healthcare team. The nurse spoke to me with great respect, explained that the treatment was safe and available for free, which reassured me a lot. She also emphasised the importance of treating my husband as well.’
Evidence-Based Change Narrative
The impetus for change originated from concerns observed in clinical practice. In healthcare units across the state of Mato Grosso, professionals reported an alarming increase in cases of gestational syphilis. Situations like these—especially when coupled with tragic, preventable outcomes such as neonatal deaths—prompted the team to seek a broader understanding of the issue.
As one nurse recounted, ‘Working on the front lines made me realise how important active listening and compassionate care are. Many pregnant women arrive feeling afraid and ashamed. When a syphilis diagnosis is confirmed, the first step is to show them they are not alone. Providing information, emotional support, and ensuring the immediate initiation of treatment is what saves the baby. I’ve witnessed cases where timely intervention prevented congenital syphilis. That gives us the certainty that our work truly makes a difference.’
Guided by this reality, the team conducted studies using the JBI methodology to assess the scope and impact of both gestational and congenital syphilis. One such study involved a scoping review of congenital infections within the STORCH+Z group (syphilis; toxoplasmosis; rubella; cytomegalovirus; herpes simplex; Zika), which revealed that congenital syphilis remained the most prevalent cause of foetal and neonatal death. Of the 32 studies included in the review, 20 were conducted in Brazil (62.5%), and 22.4% specifically addressed syphilis. Outcomes such as spontaneous abortions, foetal death, stillbirth, and neonatal death were more frequently reported in studies identifying syphilis as the primary pathogen.
Syphilis is a notifiable disease in Brazil, meaning that confirmed cases must be reported to health authorities through official notification systems. However, inconsistencies were identified in the completion of these forms, including missing or incomplete data fields, which contributed to underreporting.
The occurrence of gestational syphilis is frequently associated with low to moderate educational levels, late or inadequate initiation of prenatal care, and failure to identify and treat sexual partners. These factors contribute to vertical transmission. Moreover, delayed diagnosis and the partner’s lack of adherence to treatment compromise the effectiveness of maternal treatment, increasing the risk of progression to congenital syphilis and resulting in adverse birth conditions and low birth weight.
Demonstration of Impact
In light of this scenario, the importance of ongoing dialogue between researchers and healthcare services is emphasised, as it strengthens epidemiological surveillance through actions aimed at early identification of gestational syphilis, timely diagnosis, appropriate treatment, prevention of vertical transmission, and mitigation of harm to the newborn. The outcomes of these strategies are reflected in the indicators presented in Figure 1.
Between 2015 and 2023, reported cases of syphilis in pregnant women increased significantly—from 333 cases (3.5%) to 1,853 cases (19.5%), representing a 456.2% rise. However, although the data for 2024 are still subject to revision, a decline is observed, with 912 cases (9.64%) of gestational syphilis reported, indicating a 50.8% decrease compared to the previous year. This reduction suggests a more systematic approach to feedback in the notification system, allowing for a more accurate evaluation of the quality of care. In parallel, trends in congenital syphilis cases also reflect historical patterns of notification.
These findings underscore the need for more targeted interventions in maternal and child healthcare. In this context, nurses play a central role in care management through ongoing professional training. This includes the systematisation of the nursing process, extending from initial screening with rapid tests, monitoring of confirmed cases, and contact tracing of sexual partners, to educational initiatives that guide pregnant women on the importance of prenatal care and fostering connections with the community and family. Nurses also assist with auditing services and managing the scheduling and regulation of consultations and hospitalisations within primary healthcare.
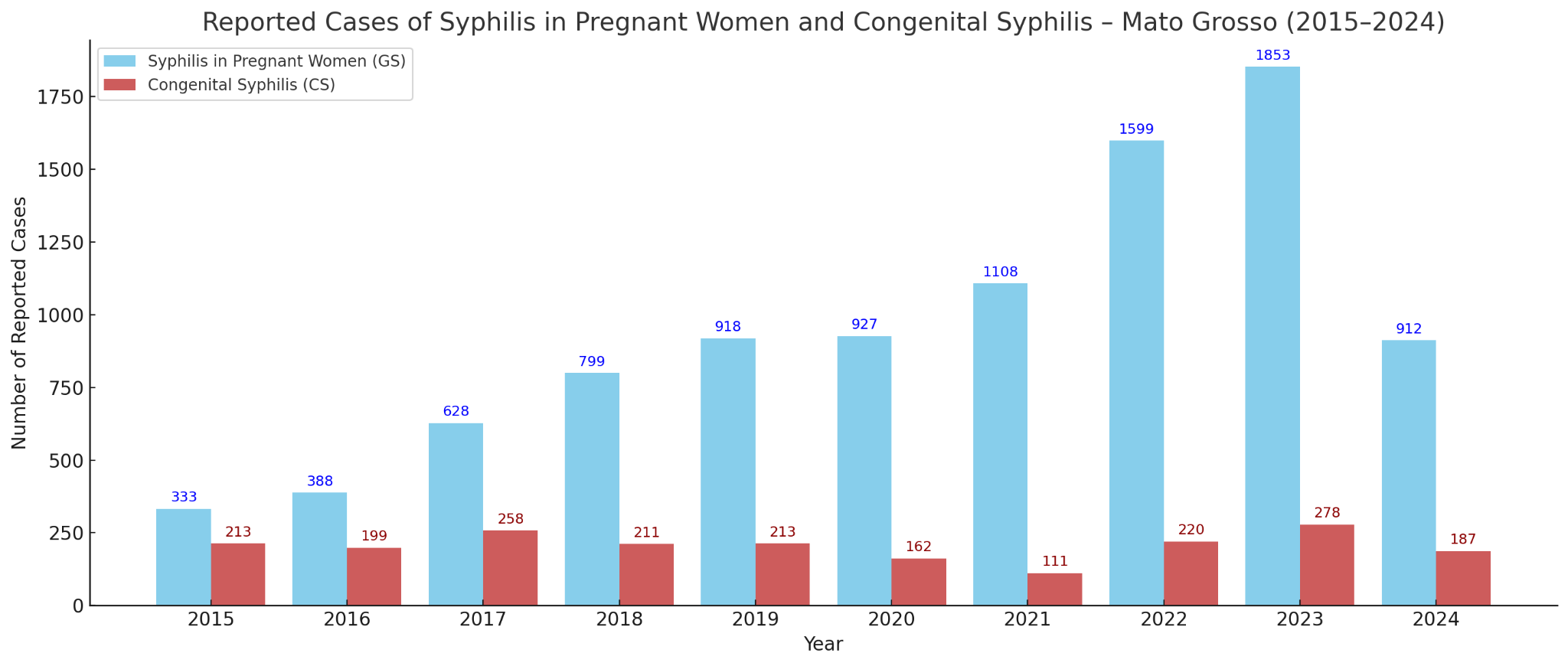
Figure 1: Confirmed cases of gestational and congenital syphilis in Mato Grosso, 2015–2024.
Source: Ministry of Health – Notifiable Diseases Information System (SINAN), 2025.
Sustainability and Future Directions
Significant progress has been achieved thus far. The next steps will aim to deepen the understanding of the subject through regional and national studies that assess the trends and impacts of congenital syphilis in Brazil, including foetal and infant mortality associated with maternal syphilis infection. Planned actions include the publication of a systematic review protocol (JBIES-24-00425), currently in press and scheduled for release on April 15, 2025. Additionally, the scope of systematic reviews will be expanded to include other outcomes, such as maternal and infant mortality, with the objective of advancing evidence-based practice grounded in more robust scientific data.
Conclusion
The experience in Mato Grosso with the use of scientific evidence—both from primary studies and systematic reviews—demonstrates that it is possible to improve syphilis surveillance and enhance the quality of care for pregnant women and newborns. Through simple measures, such as strengthening case reporting, auditing processes, and promoting integration among healthcare services, significant progress can already be observed. By leading this evidence-based approach, nursing has established itself as a key component in the prevention of gestational and congenital syphilis and in mitigating the impact of these conditions on maternal and child health.
Key Findings
In our region, the integration between clinical practice and scientific evidence still needs to be strengthened, particularly the link between academic institutions and healthcare services. The School of Nursing at the Federal University of Mato Grosso (UFMT) is the most prominent institutional force in higher education within the state and has contributed to shifting the regional epidemiological profile through initiatives such as the project presented in this article.
The findings of this study identify pathways to reinforce this connection through ongoing dialogue with municipal and state health authorities. They can also inform the planning of future interventions aimed at reducing syphilis prevalence, such as the active case finding of pregnant women and untested partners, accurate completion of notification forms, and the promotion of preventive care measures.
References
Health Surveillance Secretariat. Syphilis Epidemiological Bulletin 2024 [internet]. Brazil: Ministry of Health; 2024. Available from: https://www.gov.br/aids/pt-br/central-de-conteudo/boletins-epidemiologicos/2024/boletim_sifilis_2024_e.pdf
Primary Health Care Information System (SISAB). Prenatal indicators [internet]. Brazil: Ministry of Health; 2025. Available from: https://sisab.saude.gov.br/paginas/acessoPublico/relatorio/indicadores/IndicadorPrenatal.xhtml
Dalla Côrt JC. Congenital infections related to the STORCH+Z pathogen group in the outcomes of deaths and anomalies: a scoping review [internet]. OSF; 2023. Available from: https://osf.io/26fyu
Pan American Health Organization. Syphilis cases increase in the Americas [internet]. PAHO; 2024. Available from: https://www.paho.org/pt/noticias/22-5-2024-casos-sifilis-aumentam-nas-americas
Silva E, Silva FV, Dalla Côrt JC, Takahashi JA, Monteiro da Cruz DAL, Ferreira SMB. Incidence of adverse events and neonatal deaths related to maternal syphilis infection: systematic review – CRD42023489652 [internet]. York: Centre for Reviews and Dissemination, University of York; 2023. Available from https://www.crd.york.ac.uk/PROSPERO/view/CRD42023489652
Silva EG, Silva FV, Dalla Côrt JC, Takahashi JA, Cruz DALM, Ferreira SMB. Incidence of congenital syphilis, adverse events, and deaths in children under 2 years: systematic review protocol. JBI Evid Synth. In press 2025.
World Health Organization. Mother-to-child transmission of syphilis [internet]. WHO; 2023. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/stis/prevention/mother-to-child-transmission-of-syphilis
World Health Organization. Syphilis [internet]. WHO; 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/syphilis
World Health Organization. WHO guidelines for the treatment of Treponema pallidum (syphilis) [internet]. WHO; 2016. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384904/pdf/Bookshelf_NBK384904.pdf
Authors
Silvana Margarida Benevides Ferreira1,2, Eric Brito Ferraz2,3, Janessa Carolina Dalla Côrt2,3, Eliziani Gonçalves da Silva2,3, Camila Beatriz da Rocha2,3
1. JBI Brazilian Centre for Evidence-Based Health Care , Escola de Enfermagem da Universidade de São Paulo, São Paulo, Brazil
2. Federal University of Mato Grosso, Mato Grosso, Brazil
3. Health Department of the Municipality of Cuiabá, Mato Grosso, Brazil