Lifestyle Modification for Cardiovascular Disease Prevention
Systematic review and meta-analysis
Cardiovascular disease (CVD) remains a significant global health challenge, claiming the top spot in causes of death and disability worldwide. While strides have been made in reducing CVD mortality over the past five decades, certain populations, including racial/ethnic minorities and individuals under 65 years, still experience slow declines in rates. To address these disparities, evidence-based primary prevention strategies are crucial.
A recent systematic review and meta-analysis, published in JBI Evidence Synthesis, aimed to assess the impact of lifestyle modification on absolute CVD risk in adults with no history of CVD. The review included 29 studies with 5490 participants, focusing on interventions that exclusively utilised lifestyle modification without pharmacotherapeutics.
Six validated absolute CVD risk assessment tools were employed across the studies, including the Framingham Risk Score, SCORE, Heart Health Risk Assessment Score, Dundee, ASSIGN, and The UK Prospective Diabetes Study risk score. The pooled analysis revealed that, irrespective of the assessment tool used, lifestyle modifications consistently reduced CVD risk in the studied populations.
The lifestyle modification strategies incorporated various elements, such as diet, physical activity, motivational interviewing, psychological counselling, cardiovascular risk assessment, health education on self-management, and peer support. These interventions were employed either independently or in combination, highlighting the versatility of approaches in primary prevention.
The meta-analysis results provide compelling evidence supporting the positive impact of lifestyle modification on absolute CVD risk scores in adults without a history of CVD. The results suggest that lifestyle modification programs should entail repeated exposure.
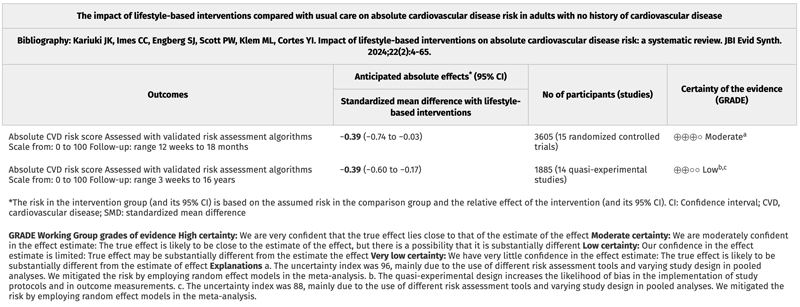
The findings of the systematic review and meta-analysis underscore the importance of consistent and reliable CVD risk assessment tools in guiding decision-making for primary prevention and facilitating comparisons across diverse adult populations.
A free access JBI Best Practice Information Sheet accompanies the systematic review and meta-analysis. JBI’s Best Practice Information Sheets are high-quality, four-page summaries of a JBI systematic review that include recommendations for practice.
A Spanish-language version of the abstract also accompanies the review and meta-analysis.
Go to the systematic review and meta-analysis in the January 2024 issue of JBI Evidence Synthesis:
Kariuki, Jacob K.; Imes, Christopher C.; Engberg, Sandra J.; Scott, Paul W.; Klem, Mary L.; Cortes, Yamnia I.
JBI Evidence Synthesis 22(1):p 4-65, January 2024. | DOI: 10.11124/JBIES-22-00356