
Community palliative care
Systematic review explores older people's perceptions and experiences
Palliative care, focusing on symptom relief at end-of-life, is essential yet inadequately accessed globally. With an ageing population, demand grows for community-based palliative care. Chronic conditions such as cardiovascular disease and cancer exacerbate this need.
Despite the World Health Organization definition and identification of quality of life domains, older adults face barriers accessing palliative care, especially at home. Community-based services are critical, reducing hospitalisation and costs, while improving satisfaction. However, research on older adults' experiences in receiving community palliative care has been lacking. A new systematic review aims to address this.
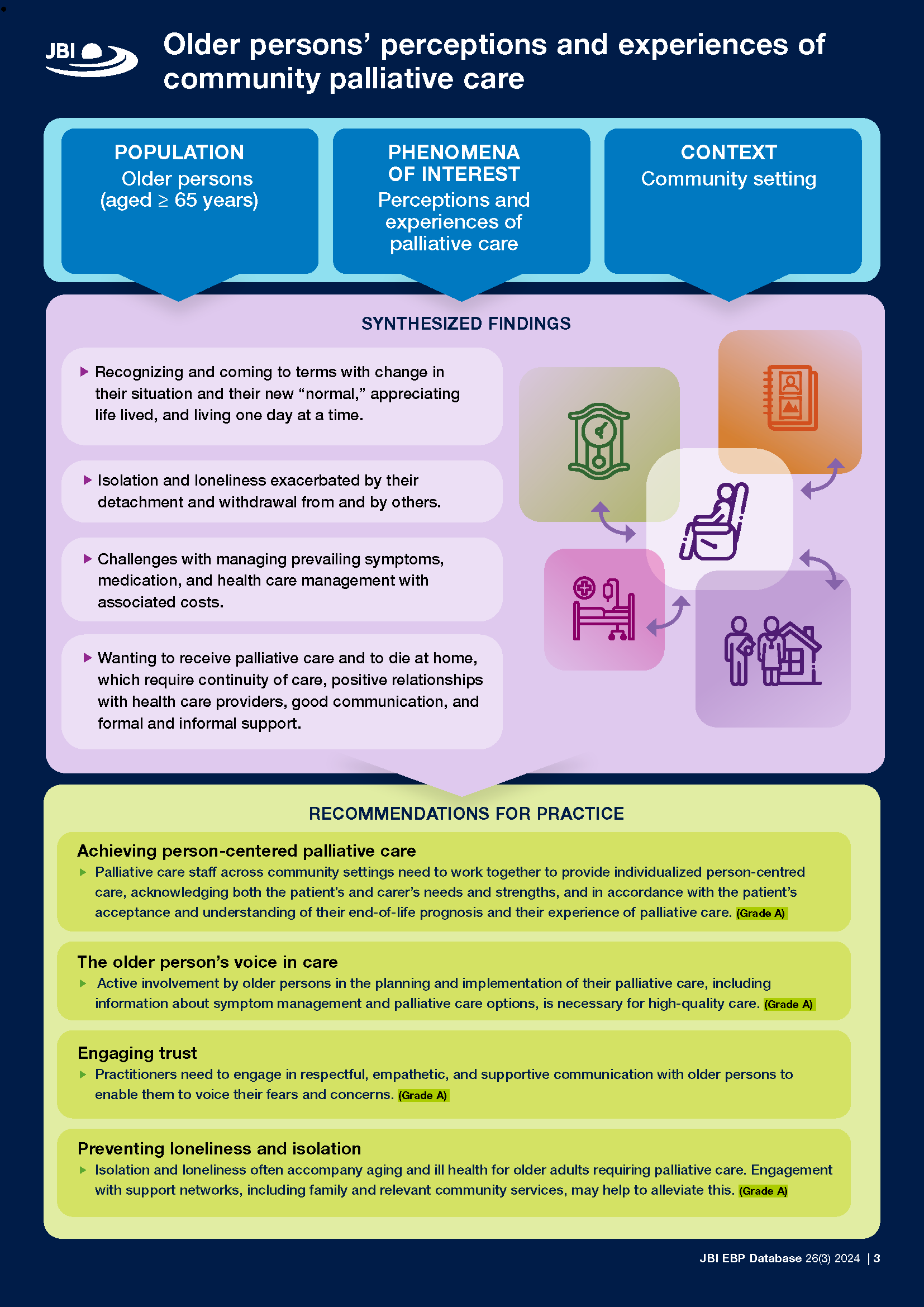
The systematic review, Older persons’ perceptions and experiences of community palliative care, examines older persons' perceptions and experiences of community palliative care, identifying four key findings:
- a redefinition of normality and appreciation for life amid significant changes;
- feelings of isolation and loneliness exacerbated by detachment from others;
- challenges managing symptoms, medications, and costs of care; and
- a desire for palliative care at home, requiring informal and formal support with continuity of care and positive relationships with healthcare providers.
Findings of the systematic review include that, despite a preference for home-based care, there is often incongruence between preferred and actual place of death due to various factors including medical needs and concerns about safety or symptom management. Advance care planning is crucial to honour end-of-life preferences, but formal support can be fragmented, lacking continuity and coordination.
The systematic review authors report that communication and relationships with healthcare providers greatly influence the quality of care received, highlighting the need for empathetic and holistic approaches to support older persons in maintaining autonomy and dignity in their end-of-life care journey.
Palliative care varies depending on the care setting, with unique challenges in community, inpatient, and acute hospital settings. Research-driven policy is essential to allocate appropriate resources, such as qualified staff, to meet the diverse needs of older persons seeking palliative care. Older individuals have the right to make choices regarding their care, emphasising the importance of their involvement in decision-making processes facilitated by effective communication among patients, families, and staff across care services.
The systematic review provides recommendations for practice such as policymaking should prioritise frameworks supporting community palliative care, including guiding principles and fostering education and collaboration among healthcare professionals to ensure evidence-based care delivery.
The systematic review is accompanied by a Best Practice Information Sheet.
The Best Practice Information Sheet provides a four-page summary of the systematic review and includes infographics and recommendations for practice.
Read the systematic review in the February 2024 issue of JBI Evidence Synthesis:
References
Cotton, Antoinette; Sayers, Jan; Green, Heidi; Magann, Linda; Paulik, Olivia; Sikhosana, Nqobile; Fernandez, Ritin; Foster, Jann
JBI Evidence Synthesis. 22(2):234-272, February 2024