Using JBI Evidence Summaries as an educational resource in a Foundations of Nursing Practice Course

June 2025
Paolo Colet, PhD, RN, RM
School of Medicine, Nazarbayev University
Astana, Kazakhstan
Paolo Colet is an Assistant Professor at Nazarbayev University, School of Medicine, in Astana, Kazakhstan.
As an educator, it is my responsibility to provide my students with the most effective learning experience possible. As an advocate of evidence-based practice, I aim to instill this mindset into my students early on in their educational journey, helping them to become safe and competent nurses in Kazakhstan. In alignment with this goal, Roussel and Thomas (2022) suggest that introducing students early to the language of implementation enables them to apply evidence-based strategies in patient care and project management. This is my story of how I introduced JBI Evidence Summaries as an educational resource into my Foundations of Nursing Practice course. To ensure ethical compliance, prior to sharing this account, I sought approval from the Nazarbayev University Institutional Research Ethics Committee, which granted me exemption status.
In 2018, I had the opportunity to participate in the JBI evidence-based clinical fellowship program at JBI, Australia. The outcomes of my fellowship were published in the JBI Evidence Implementation journal (Colet et al., 2020). However, it was not until my university subscribed to the JBI EBP Database that I realised the potential for incorporating JBI Evidence Summaries into my nursing courses, in addition to other scholarly projects. As I was reviewing my course in December 2022 and reflecting on students’ feedback, I recognised the valuable application of JBI Evidence Summaries. Furthermore, the Director of Nursing Education at Nazarbayev University has played a significant role in encouraging nursing students to think about evidence-based practice with her mantra, ‘show me the evidence’ (N. Stitt, personal communication, n.d.). This mantra, which resonated with me, became one of my favorite lines. It was these experiences that inspired me to integrate JBI Evidence Summaries into my Nursing Practice course.
In the Foundations of Nursing Practice course, students are introduced to key nursing concepts for becoming safe practitioners, with a focus on nursing skills and procedures. Alongside my teaching responsibilities, I have the duty to ensure my students stay updated with the latest evidence related to these procedures; hence, I decided to incorporate the JBI Evidence Summaries to supplement my teaching materials. Munn and colleagues (2015) define evidence summaries as a summary of the available evidence on an intervention. Petkovic and colleagues (2016) conducted a study on evidence summaries and found that their perceived usefulness and usability were of low certainty, while the ease of understanding the evidence was of moderate certainty. However, various studies conducted in different countries have used evidence summaries within a specific clinical context and found them to be effective in enhancing health professionals’ practice at the point of care (Coelho et al., 2022; Colet et al., 2020; Vedaei et al., 2023).
The Foundations of Nursing Practice course was offered to 12 second-year nursing students in the spring of 2023 over a 14-week semester, plus 1 week for examinations. The course consists of four European Credit Transfer Systems (ECTS) with a total workload of 112 hours. Specifically, the course workload can be broken down into 14 class hours, 42 laboratory hours, and 56 hours for self-study. During the first week of the course in January 2023, I briefly introduced the concept of evidence-based practice and evidence summaries to the students. We then explored our library database to familiarise ourselves with the available resources. To further align the nursing procedures taught in the course with the evidence summaries, I adopted the questions that guide the development of the JBI evidence summaries in my syllabus (Figure 1). In parallel, students were also enrolled in a medical-surgical course that included a clinical component. And so, I was thinking that this was very timely, with students making sense of the connection between what they were learning in the classroom and their experiences in the hospital. Interestingly, Roussel and Thomas (2022), argue that this teaching strategy lays the foundations for the application and integration of students’ clinical immersion, in an attempt to align evidence to their nursing care.
Upon completion of the course, students can evaluate their learning experience. There was a range of responses, with five out of twelve students ‘neither agreeing nor disagreeing’ to ‘strongly agreeing’ that the learning technologies (e.g. multimedia materials, JBI Evidence Summaries) were useful in achieving the learning outcomes of the course. Some students’ provided specific comments on the impact of using JBI Evidence Summaries:
‘They were pretty effective, but I think I was more engaging to read them online rather than on paper.’
‘They were interesting to read and proved the reliability of the methods used in specific procedures; however, I think they could have been more effective in the learning process…’
‘Well, it explains why some practices are not used and why they are not effective.’
‘It was effective as it was easier to remember specific skills due to the details I read in JBI Evidence Summaries. For example, I know that skinfold lifting during insulin administration is necessary only when the needle length is more than 4 mm. This evidence helps to remember other things about insulin: insulin is injected via a needle, subcutaneously, and there can be different needle lengths. These small details and evidence pieces help to memorise related knowledge.’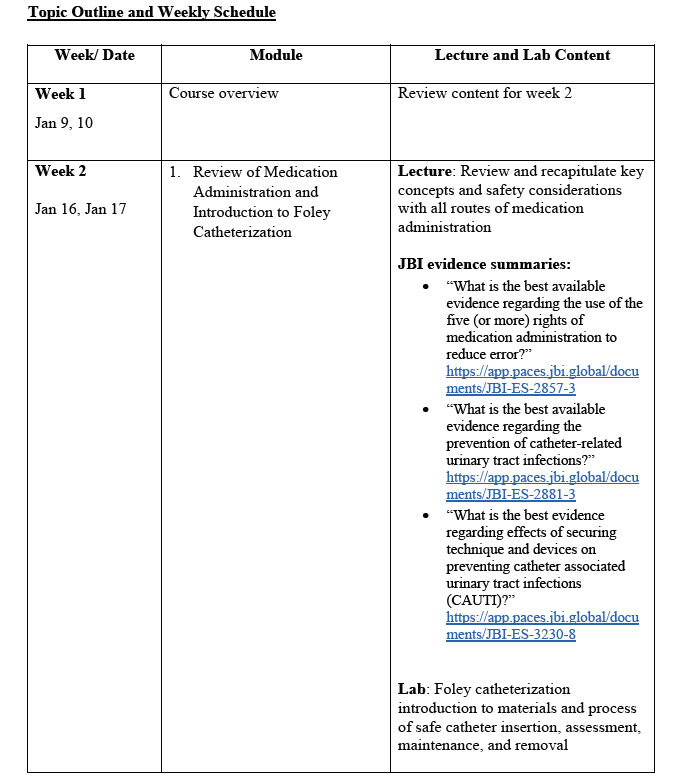
Figure 1: Extract from course syllabus
Considering both my personal experience and the students’ feedback, it seems to me that this is a promising teaching strategy. While it is still premature to draw conclusions about its effectiveness, students’ feedback indicated a positive response. However, it is important to exercise caution and acknowledge the need for formal research to test the effectiveness of this strategy in the classroom. Nevertheless, with my experience, I can say that JBI Evidence Summaries are a useful learning tool in a Nursing Practice course to introduce evidence-based practice alongside the procedures or skills that students need to learn. As a result, I will be continuing to implement these summaries into my upcoming courses.
Acknowledgements
I would like to express my gratitude to Nancy Stitt from Nazarbayev University for her feedback while writing the paper, and to my students for their responses.
References
Coelho, A., Rocha, A., Cardoso, D., Rodrigues, R., Costeira, C., Gomes, S., & Parola, V. (2022). Monitoring and management of the palliative care patient symptoms: A best practice implementation project. Nursing Reports (Pavia, Italy), 12(2), 365–370. https://doi.org/10.3390/nursrep12020035
Colet, P., Aimagambetova, G., & Kossybayeva, K. (2020). Evidence-based inpatient postnatal care among women in a national hospital in Kazakhstan: A best practice implementation project. JBI Evidence Implementation, 18(3), 318–326.
Munn, Z., Lockwood, C., & Moola, S. (2015). The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach. Worldviews on Evidence‐Based Nursing, 12(3), 131–138.
Petkovic, J., Welch, V., Jacob, M. H., Yoganathan, M., Ayala, A. P., Cunningham, H., & Tugwell, P. (2016). The effectiveness of evidence summaries on health policymakers and health system managers use of evidence from systematic reviews: A systematic review. Implementation Science, 11(1), 1–14.
Roussel, L. & Thomas, P. (2022). Implementation science in nursing: A framework for education and practice [Kindle edition]. Slack.
Vedaei, A., Iranmanesh, P., Tahani, B., Mostafaei, A., & Talebpour, A. (2023). Promoting oral and dental healthcare among the elderly in a residential care home in Isfahan: A best practice implementation project. JBI Evidence Implementation, 21(1), 25–35.