Using JBI Evidence Summaries
June 2025
Madeleine Whalen, Johns Hopkins Health System, USA
The Johns Hopkins Health System (JHHS) is an academically based group of hospitals that consists of five hospitals in the Midatlantic region and one children’s hospital in the Southern United States. Like many hospitals in the US, JHHS onboards hundreds of new nurses each year through a program called Nurse Residency. Although our hospital system produced and maintains the Johns Hopkins Evidence-Based Practice (EBP) for Nurses and Healthcare Professionals Model and Guidelines, each affiliate has a wide range of resources and experience in EBP.
Nurse Residency Programs are structured year-long offerings that have been shown to improve nurse retention and help nurses make the transition from student to professional nurse. Traditionally, one component of the Nurse Residency Program is the completion of an EBP project. Unfortunately, these projects have been fraught with a variety of issues, including lack of time and resources to complete a robust and actionable EBP project. The evidence included tended to be piecemeal and not reflective of the true state of the literature on a topic. Additionally, many of the topics were not well-suited for an EBP approach and there was no way to validate the residents’ skill acquisition. The JBI Evidence Summaries offered a solution by providing actionable recommendations based on sound methodology.
In July 2022 our health system implemented a new EBP curriculum for nurse residents. While the overall goal of the content is to foster the spirit of inquiry by establishing foundational knowledge regarding EBP and how it applies to the learners as professional nurses, a secondary aim was to understand available resources, including the JBI EBP Database. Didactic content includes a tour the organization’s library site and navigation to the JBI webpage and case studies are structured around a JBI Evidence Summary. See Figure 1 for details of the case study process that uses both the Johns Hopkins EBP process and JBI resources.
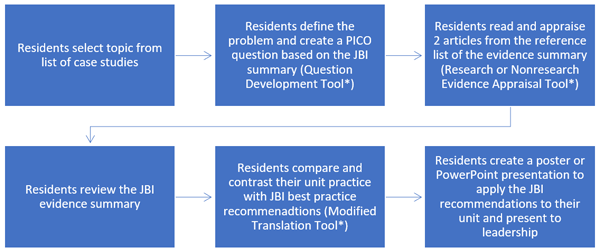
Case studies include pdfs or print-outs of the JBI Evidence Summary and answer keys to all relevant Johns Hopkins EBP tools. To encourage adoption of the recommendations, presentations to leadership include highlighting the gap between current and best practice, data to gather and stakeholders to engage. This approach has helped to reinforce the true scope of the EBP project as well as created tangible and actionable recommendations that can be put into action of the unit level. It has additionally off-loaded some of the burden on educators to create content and impart EBP principals without drawing the complete picture. Resident feedback has included:
“Great class that combined many elements for best practices”
“Learning more about EBP, QI [quality improvement] and research will be helpful moving forward in my career as well as out project”
“Both fun and great academic learning experience”
“Helps me ask “why” we do certain things in nursing”
“It will help me be aware of how to identify EBPs and QIs in my nursing and prevent me from making errors in my care”
“Introduction to EBP made me understand more of what goes into investigation and improvement”
“It’s a nice way to develop knowledge and understanding of how to create EBP”

While the new curriculum and case studies have provided evidence-based recommendations that represent low-hanging fruit for units or departments, there is a gap between generating recommendations and implementation because the projects are completed at the end of the one-year residency. We are actively looking for ways to ensure clinical practice continually reflects the best evidence beyond the residency program. We have also had some difficulties throughout the case study process with larger groups. Because this is a multi-step process that merges two approaches (JBI and Johns Hopkins EBP Model), there is a need for a significant amount of guidance and explanation throughout the project. This is improving as the educators become more familiar with the workflows but can be continually improved.